You likely manage vast amounts of information every day. From resident medications to dietary requirements, the volume of data in the care sector is massive. However, a significant problem exists in how this information moves between systems. Often, it does not move at all. This is where aged care interoperability becomes the primary focus for the future of the industry.
Interoperability refers to the ability of different computer systems and software to communicate, exchange data, and use the information that has been exchanged. According to a recent report by the Australian E-Health Research Centre (CSIRO), the current landscape relies heavily on manual processes. Many providers still send information via fax, email, or paper documents. This approach creates risks for errors and slows down care delivery.
This article examines why connecting these systems is necessary and how new standards will change the way you work.
Key Takeaways
- Siloed Data: Current systems often trap data, which forces staff to enter the same information multiple times.
- Standardization: Adopting common languages like FHIR allows different software to speak to each other.
- Safety: Better data flow reduces medication errors and improves resident safety.
- Efficiency: Automating data transfer frees up time for direct care.
The Current Data Landscape
The CSIRO report on the Aged Care Data Landscape highlights a fragmented system. You might recognize this in your own operations. Information often sits in "silos." This means the clinical software does not talk to the medication management system, and neither talks to the government reporting portal.
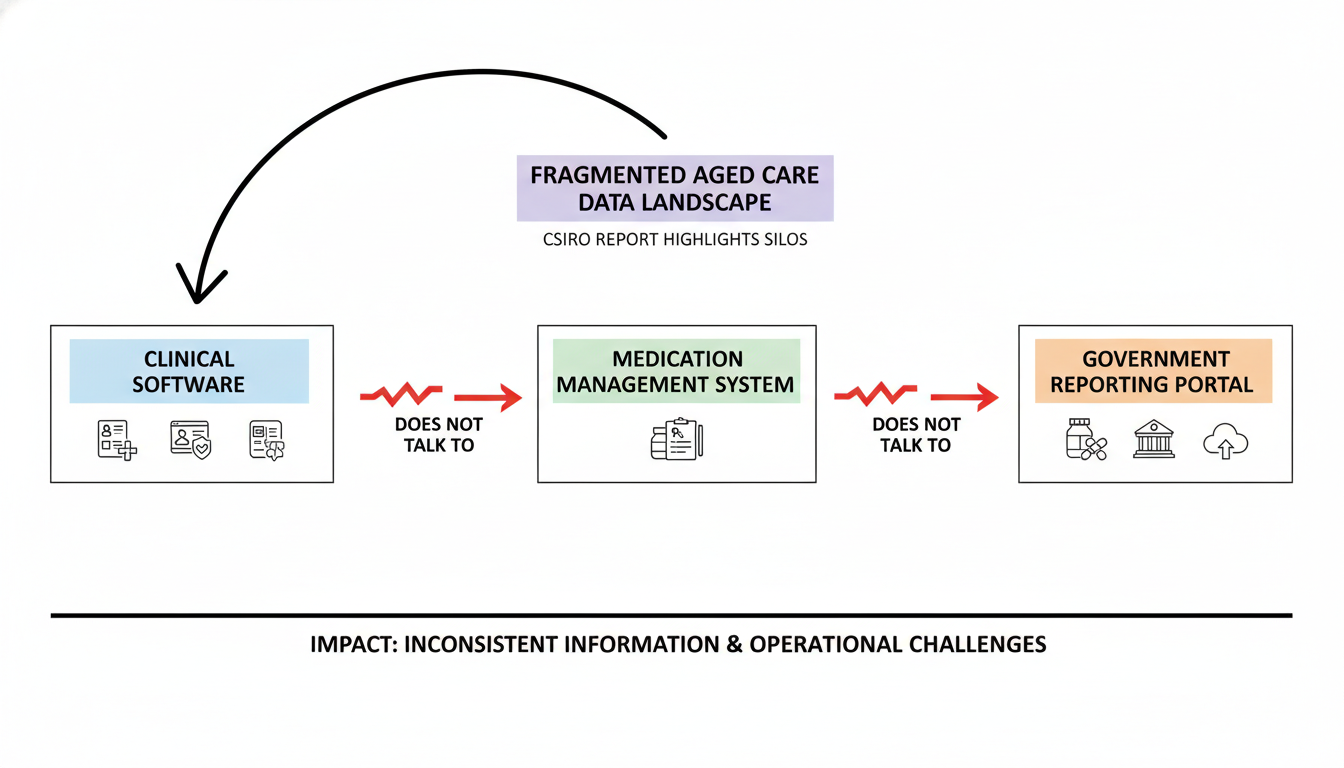
This fragmentation causes several specific issues:
- Duplicate Entry: Staff members must type the same resident details into three or four different platforms.
- Inconsistent Records: If a change happens in one system but is not updated in another, the records disagree.
- Administrative Burden: Time spent on manual data entry takes away from time spent with residents.
- Transfer Risks: When a resident moves to a hospital or a new facility, their data often does not travel with them effectively.
The industry must move away from document-based exchange (like sending a PDF) toward true data exchange. In a data-based model, specific pieces of information—like a blood pressure reading or an allergy—move directly between databases without human intervention.
Why Digital Health Standards Matter
To fix fragmentation, the industry needs rules. These rules are called digital health standards. Think of them like the grammar and vocabulary of a language. If two people speak different languages, they cannot understand each other. The same applies to software.
Without standards, Vendor A organizes data one way, and Vendor B does it differently. Standards provide a common framework so that:
- Structure is Uniform: Everyone agrees on how to format a date of birth or a diagnosis code.
- Terminology is Consistent: Everyone uses the same codes for medicines and treatments.
- Security is Maintained: Everyone follows the same protocols to keep data safe during transfer.
Adopting these standards removes the guesswork for software developers. It allows your organization to choose the best tools for each job, knowing they will work together.
The Role Of FHIR In Data Exchange
One specific standard stands out in modern healthcare: Fast Healthcare Interoperability Resources, or FHIR (pronounced "fire"). This framework is the modern standard for exchanging healthcare information electronically.
FHIR is different from older standards because it is built for the web. It is easier for developers to implement and works well on mobile devices.
How FHIR Supports You
- Granular Data: Instead of sending a whole document, FHIR allows you to send specific "resources," like a single prescription or a lab result.
- Real-Time Access: It supports real-time queries. A doctor can pull up a resident's current medication list instantly.
- Flexibility: It can handle various types of clinical and administrative data.
The CSIRO report emphasizes that moving to FHIR is a necessary step for the sector. It creates the foundation for a responsive and accurate health system.
Understanding The Sparked Program
In Australia, the push for better data connection is organized under the Sparked program. This initiative brings together government, software vendors, and care providers to design the core data standards for the industry.
The Sparked program focuses on defining exactly what information needs to be shared and how. Their work includes:
- Clinical Data Definitions: Deciding exactly what constitutes a "transfer of care" summary.
- Technical Guides: Writing the technical manuals that software vendors use to build their products.
- Testing Events: Holding "connectathons" where vendors test if their software can actually talk to each other.
By following the guidance from Sparked, the sector moves toward a unified approach rather than every provider trying to solve the problem alone.
Benefits Of Connected Care Systems
When you achieve connected care, the benefits extend beyond just the IT department. It fundamentally changes the daily experience for staff and residents.
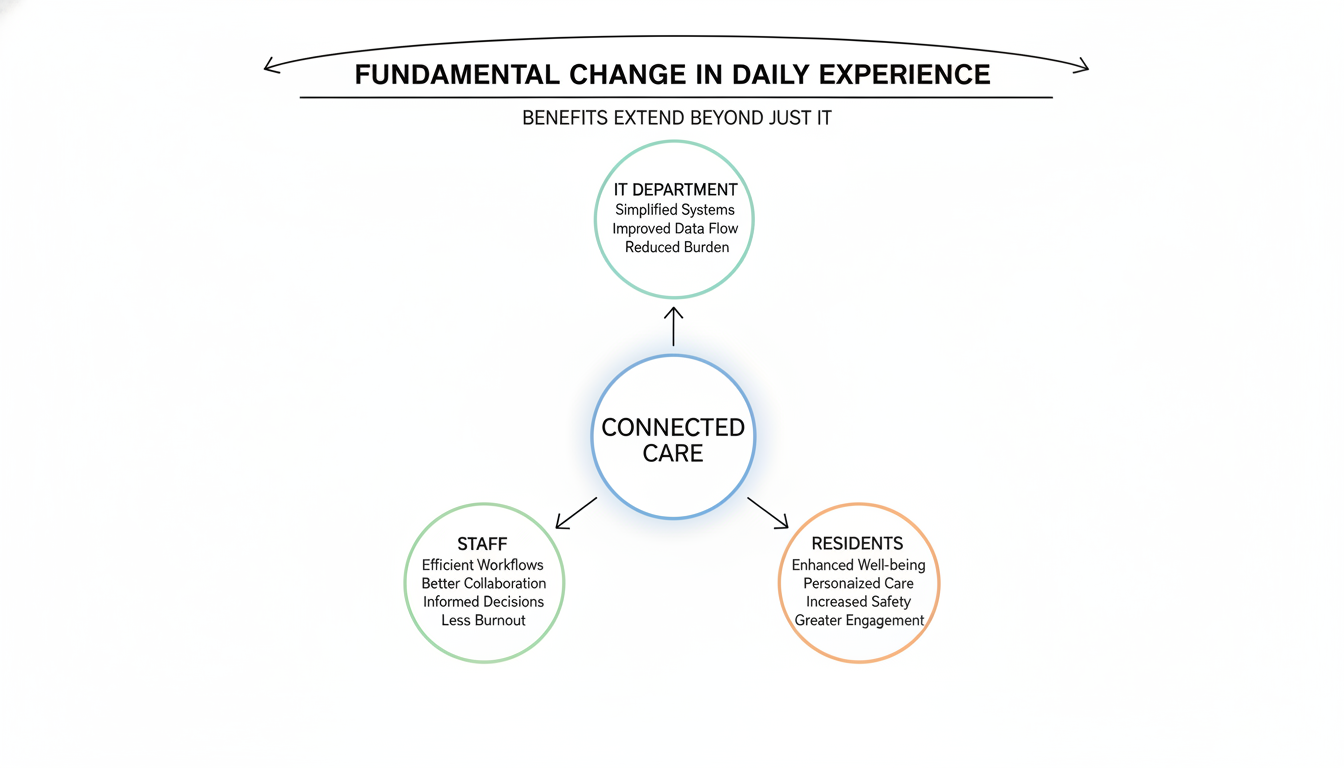
Operational Improvements
- Reduced Admin Time: Automated transfers mean less typing and copying.
- Faster Admissions: When a resident arrives, their data can populate your system automatically.
- Better Reporting: accurate data makes mandatory government reporting easier and more precise.
Clinical Improvements
- Medication Safety: Pharmacists, GPs, and facility staff view the exact same medication list. This reduces the risk of incorrect dosing.
- Holistic Views: Care teams can see a complete history, including hospital visits and allied health notes.
- Improved Transitions: When a resident goes to the hospital, the hospital receives their history immediately. When they return, you receive their discharge summary instantly.
Key Challenges To Implementation
While the future looks promising, you must acknowledge the hurdles. Transitioning to a fully interoperable system takes time and resources.
- Legacy Systems: Many providers use older software that was not built for modern data exchange. Upgrading these systems can be expensive.
- Data Quality: If your current data is messy or incomplete, sharing it will not help. You must clean up existing records first.
- Privacy Concerns: Sharing data requires strict consent models and security measures to protect resident privacy.
- Change Management: Staff need training to use new workflows. They must understand why the new process is better than the old paper forms.
The CSIRO report suggests that while these barriers are real, the cost of doing nothing is higher. Staying with manual processes will only become more difficult as the population ages and care needs become more complex.
Frequently Asked Questions
What is the difference between integration and interoperability?
Integration usually refers to connecting two specific systems, often with a custom link. Interoperability is broader; it means systems can communicate using shared standards, allowing many different systems to connect without custom work for each one.
Why is the sector moving away from PDF documents?
PDFs are digital paper. A computer cannot "read" the medical data inside a PDF to check for drug interactions or graph trends. Structured data allows computers to process the information to help clinical decision-making.
Do I need to replace all my software?
Not necessarily. Many software vendors are updating their existing products to support standards like FHIR. You should ask your current vendors about their roadmap for interoperability.
Preparing For A Connected Health Ecosystem
The transition to a connected aged care environment is underway. The insights from the CSIRO report make it clear that aged care interoperability is not just a technical upgrade; it is a requirement for sustainable care.
By prioritizing digital health standards and supporting initiatives like the Sparked program, you position your organization for success. The goal is a system where data flows freely and securely, allowing your team to focus on what matters most: providing excellent support to residents.
You should begin by auditing your current systems. Identify where data enters a dead end. Talk to your software partners about their plans for connection. The future of care is connected, and preparing for it now will provide stability and efficiency for years to come.


.png)
.png)



