The Difference Between Priority 1 and Priority 2 SIRS Incidents
For organizations operating within the aged care sector, understanding the Serious Incident Response Scheme (SIRS) is fundamental to accountability and resident safety. A critical aspect of SIRS is recognizing and correctly categorizing reportable incidents as either Priority 1 or Priority 2. Misidentifying the severity or reporting tier of an event can lead to missed deadlines and non-compliance, compromising both regulatory standing and the well-being of those receiving care.
This writing serves as a technical discussion to clarify the distinctions between these two reporting tiers and the strict timelines associated with each.
The Serious Incident Response Scheme (SIRS) Framework
SIRS establishes a consistent approach for managing and reporting serious incidents in aged care. Its main objective is to reduce the risk of harm to older persons and promote a culture of transparency and continuous improvement among providers. When an incident occurs, staff must quickly assess its nature to determine if it is reportable and, if so, its priority level.
The priority level determines how quickly the incident must be reported to the Aged Care Quality and Safety Commission. The severity and impact on the person receiving care are the main factors driving this classification.
Priority 1 Incidents: Immediate Action Required
A Priority 1 reportable incident signifies an event of high severity that requires the most urgent attention and notification. These incidents usually involve significant harm, the potential for serious harm, or specific, serious types of misconduct.
Examples of incidents typically classified as Priority 1 include:
- Serious Physical or Psychological Harm: An incident that causes a physical injury or psychological distress so severe that it necessitates medical intervention or specialist psychological treatment. This moves beyond minor, expected bumps or scrapes and into the territory of genuine injury requiring professional care.
- Unlawful Sexual Contact or Inappropriate Sexual Conduct: Any instance of non-consensual sexual activity or boundary violations that constitute inappropriate sexual behavior.
- Unexpected Death: The death of a person receiving aged care services that was unexpected or related to an incident.
- Unexplained Absence: When a person receiving aged care services goes missing and there are solid reasons to involve law enforcement (the police). This is sometimes referred to as 'unexplained absence.'
The Reporting Timeline for Priority 1 Incidents
The need for speed in reporting a Priority 1 event is absolute. The law mandates that providers must report Priority 1 incidents to the Commission within 24 hours of becoming aware of the incident. This is a very tight window, emphasizing the seriousness of the event.
Furthermore, if the provider cannot supply all the necessary information at the time of the initial 24-hour notification—perhaps because a thorough investigation is still underway—any outstanding details must be provided to the Commission within the following five days.
This 24-hour timeframe is not merely an administrative requirement; it is a mechanism designed to help the Commission monitor critical situations and potentially intervene swiftly to protect other individuals or to ensure the provider is taking adequate measures. Missing this deadline is a serious compliance failure.
Priority 2 Incidents: A Different Type of Reportable Event
Priority 2 reportable incidents cover all other reportable incidents that do not meet the definition or severity requirements of a Priority 1 incident. This does not mean these events are unimportant; rather, their immediate impact or severity is categorized as less severe than a Priority 1 event, thus allowing a longer period for internal response and external reporting.
A common definition for a Priority 2 incident is: any reportable incident that did not result in death, serious injury, or major harm requiring immediate medical or psychological treatment, and is not an unexplained absence or sexual misconduct that would qualify for Priority 1.
The reporting requirements for Priority 2 incidents acknowledge that while the incident is significant enough to be reported under SIRS, it allows the provider more time to investigate and compile a thorough report.
The Reporting Timeline for Priority 2 Incidents
Providers must report Priority 2 incidents to the Commission within 30 calendar days of becoming aware of the incident.
This longer timeline gives providers the space to conduct a complete internal review, gather all relevant facts, assess what went wrong, and document the corrective actions taken before submitting the final report. This detailed documentation is a key part of the quality improvement cycle within SIRS.
The Decision-Making Process: Priority 1 vs. Priority 2
Deciding whether an incident is Priority 1 or 2 often requires judgment, particularly when determining the degree of harm.
If an incident involves alleged abuse or neglect, and the result is anything that requires professional medical or mental health care, it moves directly into the Priority 1 category. If, however, the harm is minor and temporary, or if the event is a type of reportable incident (like theft) that does not cause serious injury, it is more likely to be a Priority 2 event.
A good rule for staff members who are unsure is: When in doubt, treat it as Priority 1. It is far better to report early and over-classify an incident than to under-classify it and miss the 24-hour deadline. Service managers must make sure workers are well-trained in applying these classification rules.
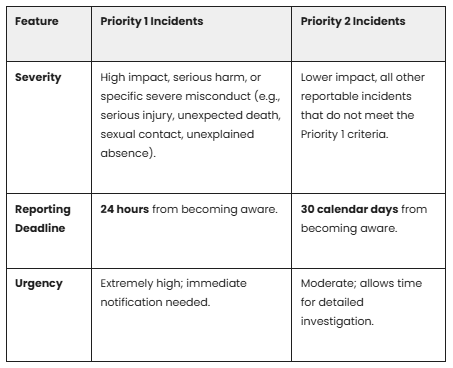
Key Differences Summarized
The Importance of Accurate Reporting
Adherence to these reporting timeframes is more than just following the rules; it is about accountability for the quality of care provided.
- Compliance: Failing to report an incident within the correct timeframe can result in sanctions or regulatory action from the Commission.
- Safety: Quick reporting of Priority 1 events allows the regulator to monitor the situation, confirming that immediate steps are being taken to protect other individuals and address systemic problems.
- Learning: Accurate and timely reporting feeds into the national system, helping providers and the Commission identify trends and systemic risks across the aged care sector.
In both instances, the provider must also notify the Commission of any major new information about a reported incident as soon as reasonably practical after becoming aware of the information, even after the initial report has been filed. This means the duty to inform the regulator continues beyond the initial submission.
Mastering these reporting tiers and their associated deadlines is a fundamental responsibility for every aged care provider. It demands a robust internal system for incident detection, assessment, and notification, making sure that when serious events occur, the response is swift, correct, and compliant with SIRS requirements.
Frequently Asked Questions (FAQs)
Q: What is a "reportable incident" under SIRS?
A reportable incident is an event that falls into one of the categories defined under the SIRS laws, such as unreasonable force, neglect, unexplained absence, certain types of theft, or inappropriate restraint.
Q: Does SIRS apply to all aged care services?
SIRS generally applies to residential aged care providers and certain in-home care services that receive funding from the government.
Q: What if I am unsure if an incident is Priority 1 or Priority 2?
If there is any question about the severity or classification of an incident, the safest course of action is to treat it as a Priority 1 incident and report it within the 24-hour timeframe. You should consult with the service manager immediately.
Q: What happens if we miss the 24-hour reporting deadline for a Priority 1 incident?
Missing the deadline is a serious failure of compliance. It must still be reported immediately, and the Commission may ask for an explanation as to why the timeline was not met. Consistent failure to meet reporting deadlines can lead to regulatory action.
Q: Do we need to finish the investigation before reporting a Priority 1 incident?
No. You must report a Priority 1 incident within 24 hours of becoming aware, even if the internal investigation is not finished. You then have five additional days to supply any missing information.
Q: If a Priority 2 incident later gets worse, does the classification change?
Yes. If new information suggests the harm caused by a reported Priority 2 incident is more serious and meets the criteria for Priority 1, the provider must update the Commission with the significant new information as soon as reasonably practical.
Q: Who should be notified internally when an incident occurs?
The process usually begins with frontline staff reporting to a supervisor or manager who is designated to handle SIRS assessments and reporting to the Aged Care Quality and Safety Commission. Providers must have clear internal policies for this communication chain.
Q: Does the person receiving care or their family need to be informed of the report?
Yes, providers are usually required to notify the person affected and/or their representative about the reportable incident and the actions being taken, unless doing so would put the person at risk of harm.
Q: Where can providers find the most current guidance on SIRS?
The Aged Care Quality and Safety Commission publishes detailed guides and technical specifications that service providers should check regularly for updates.


.png)
.png)



